Podcast: Play in new window | Download (Duration: 16:58 — 15.5MB)
Subscribe: Apple Podcasts | RSS | More

You are called down to your HDU to review a 81 year old woman who is day one following a major laparotomy for ovarian cancer surgery. The nursing staff are worried because “she is not quite right”. She hasn’t made much urine over the last 3 hours, her blood pressure is a little low and she has also developed low peripheral oxygen saturations on room air and is now needing 3l/min via nasal prongs. She had a unit of blood earlier this morning and has had 4-5 litres of intravenous fluid now both during and after her operation.
What to do?
Should you give her a 500ml bolus of fluid to help her urine output and maybe boost her BP a little? But why are her saturations low – what if you push her into florid pulmonary oedema? Why are her sats low? Does she have pleural effusions? atelectasis? early pulmonary oedema? Should you give her a vasopressor? some frusemide? some physio? some more fluids? Aaarrgggh!
You get out your stethoscope – her lungs are quiet at the bases and she is slightly breathless but you are still not sure what’s going on. You move your stethoscope to teh middle of her chest and you can’t hear any murmurs – but this doesn’t really tell you that there is nothing wrong with her heart or valves for that matter!. Oh well at least you had a couple of quiet minutes without talking to the patient or nurse to think about what you might do next !
Only 10m away in the corner of the unit you spot the portable USS machine, which has a curvilinear and phased array probe. You remember the talk from your colleague last week on point of care USS. They described how in around 5min you could probably confidently answer most of these questions & you make a mental note that you are definitely going to sign up for that course in 2 months time…
Hi Everyone,
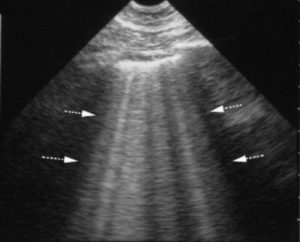
Welcome to this weeks podcast episode where Dr Parvesh Verma and I discuss the pros and cons of lung ultrasound and the vastly under utilised potential of this relatively easy to perform bedside technique. Lung ultrasound is relatively easy to learn, is vastly more accurate than lung auscultation, quite a bit better than CXR and as good as invasive radiation heavy investigations like chest CT.
In just about every clinical setting we all have access to an ultrasound machine now. If you ever listen to someone’s chest or look after patients with dyspnoea (in hospital or a clinic ) then hopefully this episode will inspire you to go away and learn this incredibly useful skill!
Merry Xmas & Happy New Year! This will probably be the last episode this month – I am keen to get suggestions on topics for future episodes so please send me all your suggestions and great ideas!
References / Links
There are a huge number of free resources out there to introduce you to this topic – please search for them yourself. The links below are not necessarily the best but you might find them useful:
- Practical Guide to Lung Ultrasound BJA Education – free article
- Lung ultrasound compared with chest X‐ray in diagnosing postoperative pulmonary complications following cardiothoracic surgery: a prospective observational study†
- BMJ – Lung ultrasound: a useful tool in the assessment of the dyspnoeic patient in the emergency department. Fact or fiction?
Youtube Tutorial
A short video tutorial is one of the best ways to introduce yourself to the basics of lung ultrasound. Therea re a large number of video tutorials on this topic – choose your own favourite! Here are a couple which I thought were good:

3 thoughts on “044 – Lung ultrasound a discussion with Dr Parvesh Verma”
The podcast will not play
Thanks Kathryn – Glitch is now fixed!
Thanks Roger