Podcast: Play in new window | Download (Duration: 32:57 — 30.2MB)
Subscribe: Apple Podcasts | RSS | More
(Real Case: De-identified)
You receive a call from a frantic ward nurse who tells you they have a 32 yr old woman who had laparoscopic surgery for treatment of endometriosis earlier in the day and she is in severe pain despite having had 3 doses of sublingual buprenorphine and 4 doses of tramadol since theatre 4 hours earlier. You head up to the ward and read her notes – she has had chronic pelvic pain since a teenager, she has been on analgesic drugs chronically for many years and been managed by her GP and a chronic pain service. She has a history of anxiety and depression and sexual abuse as an adolescent. Her current preoperative regimen involved tapentadol SR, amitriptyline, celebrex, pregabalin and prn oxycodone. In theatre she had a volatiel anaesthetic and a number of multi-modal analgesic medications including a small dose of methadone, ketamine, lignocaine. She needed a lot of fentanyl in recovery and since arrival on the ward has been very hard to control. You go and see her, she is definitely not narcosed from all these drugs! She is wide awake, slightly tachycardic (HR 105), restless and complaining of diffuse abdominal pain. She says “Doc it’s 11/10” and is asking for you to give her something else to help please!
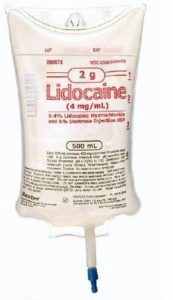
You talk her about your options then decide together to admit her to your HDU for overnight intravenous lidocaine infusion. She has the 100mg loading dose over 10min then is started on a 1mg/kg/hr infusion. Within 2 hours she is asleep and when you see her in the morning she says her pain is only 3/10 and she thanks you profusely….
Hi this week on the podcast we are joined by my colleague Dr Kevin Chan and we discuss the pros / cons of intravenous lidocaine infusions and it’s increasing use in perioperative pain management!
Previous Podcasts
The Opioid Epidemic a discussion with Dr Sonia Ting
References
Podcast with author from the above article: Their experience at Ottawa Hospital

3 thoughts on “037 – Intravenous lidocaine infusions for analgesia with Dr Kevin Chan”
I was contacted by Casey Parker with two great questions which I think will be of interest to other listeners/ readers so I have posted my responses to them here:
1. Why Lidocaine versus lignocaine ?
The TGA are mandating that we change our names of certain medications over the next 4 years to be consistent with international naming practices.
http://www.tga.gov.au/updating-medicine-ingredient-names-list-affected-ingredients
2. Casey had a patient with perioraltingling after injecting only 1.5ml of iv lidocaine 1% when trying to soothe an uncomfortable iv site – this made him concerned she was developing toxicity and so he decided not to go with iv lidocaine infusion.
I have also had this described to me by patients too if you inject the loading dose to them when fully awake – I am guessing it’s related to the speed at which it’s transported from the arm to the brain snd the speed it redistributes. When giving the loading dose to awake patients it is better to do it really slowly over 5-10min. When I give it at the start of an anaesthetic now I inject the lidocaine as the propofol goes in – ie over about a minute, kills two birds with one stone, stops the propofol sting and gets the loading dose in, but after they are sedated / unconscious. I am sure that if they weren’t being rendered unconscious they would probably complain about some perioral tingling. I have literally used iv lidocaine in hundreds of patients- as have my colleagues and giving 70-100mg to a 70-90kg adult over a few minutes at the start of the ga after they’re asleep is very safe.
In regards to using lidocaine to soothe the iv site or prevent the arm ache from propofol induction: if I’m concerned I often do an amateur biers block – I circumferentially tourniquet their arm (using my grip or an actual tourniquet) and inject 3-5ml of the lidocaine with the drip off. I keep this manual tourniquet on for 60-90s to try and get everything nice and numb. Interestingly when I release this I thought I would also get patients describe perioral tingling etc but seems much less of an issue..
Great questions!
Worst induction experience ever. I had a complete panic as the lidocaine hit the brain. Never again. I asked around, other doctors had the same experience
Thanks Andrew for your feedback, not sure how the lidocaine was administered in your case obviously but you raise an important point. I can’t remember how we discussed it in this podcast now (it is a few years old) but a good reminder that a bolus of lidocaine in awake people can be unpleasant! We should administer the loading dose of lidocaine very slowly if someone is awake (e.g. starting it in PACU or an HDU) or in the case of giving it at induction perhaps give most of it after they lose consciousness…I still find giving some lidocaine simultaneously as you start the propofol is very useful to prevent the pain from the propofol – which I have also been told many times is equally a horrible experience for some!