Podcast: Play in new window | Download (Duration: 24:15 — 22.2MB)
Subscribe: Apple Podcasts | RSS | More
(*Hypothetical patient)
You are called to review a woman who recently arrived in your hospital and is now a few hours postpartum after a pre-term vaginal delivery at 35 weeks. She tells you that she has felt unwell for the last few days with a little bit of vomiting, diarrhoea and her asthma has been playing up and needing quite a few puffs of her ventolin. She went into preterm labour and delivered quickly 2-3 hours ago. She has received 3-4 litres of crystalloid to treat her “dehydration” and the at times non reassuring CTG over the last 24hours. She isn’t febrile, but is tachycardic at 115/min, hypotensive 95/45 and she looks a little short of breath with Sp02 92% on room air and a respiratory rate of 20/min. She can talk in sentences and is walking around her room so you are reassured by this. After taking a history and examining her you decide to have a quick look at her heart and lungs with your USS machine (you have recently completed a point of care ultrasound course so are always looking for an opportunity to put your new skills into practice).
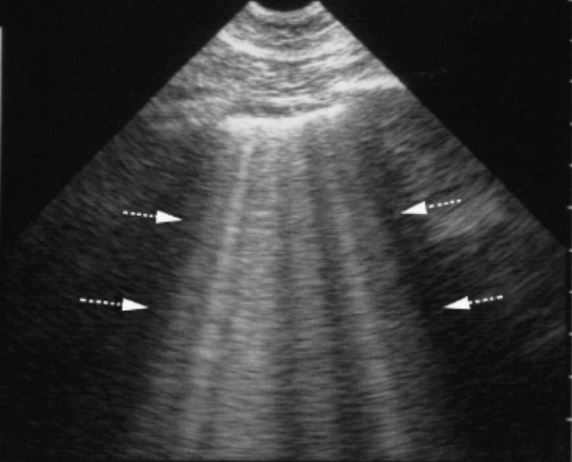
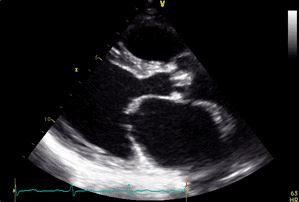
To your surprise you discover the apices of both her lungs have a large number of B-lines and then when you throw the probe on her heart and inferior vena cava within a couple of minutes you see she has a large poorly contracting left ventricle and a dilated IVC. You reach over and turn off her iv fluids – this woman doesn’t need anymore rehydration!
Hi everyone,
This week Parvesh and I follow up on our earlier podcast discussing the utility of point of care lung ultrasound with a discussion about the merits of point of care echocardiography. Join us and as we discuss the pros / cons, share some anecdotes and talk about where we are on our journey learning this incredibly useful new technique.
Links
These articles are not free open access – they are available through most university / hospital libraries or your medical college (eg ANZCA).
